Commonly Treated Conditions
Hypertension

Also known as "High Blood Pressure", hypertension is a potentially serious condition which can lead to other cardiovascular diseases such as coronary artery disease, heart failure, kidney disease, and stroke. More than 70 million Americans have hypertension, mostly without symptoms.
Blood pressure is the force of blood exerted on the walls of blood vessel during circulation. In general, blood pressures at rest above 140/80 mmHg is considered high. Systolic blood pressure (the upper number) is the pressure during the beating of heart, and diastolic blood pressure (the lower number) is the pressure during the relaxation of heart between the beats. If it remains elevated over time, many potentially serious bodily damages may occur. By adopting healthy lifestyle habits and following proper treatment plan prescribed by your healthcare providers, many of the hypertension-related complications can be prevented.
Hypercholesterloemia

Cholesterol is a fatty substance made in the body and is also present in some foods we eat. While cholesterol is a necessary part of normal bodily function, its excess build-up in the blood can lead to coronary artery hardening with blockages called atherosclerotic plaques. If this reaches a severe condition, one can suffer symptoms such as angina (chest discomfort induced by severe coronary artery blockage), heart attack, or stroke.
It is desirable to keep total cholesterol below 200 mg/dl, LDL cholesterol (low density lipoprotein - the "bad" cholesterol) below 130 mg/dl in general, below 100 if you have other risk factors, and below 70 if you have established coronary artery disease. The HDL cholesterol (high density lipoprotein - the "good" cholesterol which helps cleanse the bad ones) above 40 mg/dl is considered good, but preferably above 60 for better protection against developing cardiovascular disease.
If you have risk factors(s) to develop heart disease or stroke, such as cigarette smoking, diabetes, high blood pressure, obesity or family history of heart disease, periodic blood tests of your cholesterol profile is highly recommended. Healthy diet low in saturated fat, regular exercise, and weight loss can help lower cholesterol. When these measures are not enough, adding a cholesterol-lowering medicine(s) under the supervision of your doctor may be necessary in order to improve your cardiovascular health.
Coronary Artery Disease
More than 17 million people in the U.S. suffer from coronary artery disease (CAD), making it the most common form of heart disease. Coronary arteries are small blood vessels that supply blood and oxygen to the heart muscle. If the arteries develop atherosclerotic plaque due to excess fatty deposits, the blood flow to the heart muscle can be reduced, causing a variety of symptoms.
These include chest pressure, pain, or burning, arm, jaw, or neck discomfort, unusual shortness of breath, irregular heart beats, dizziness, unusual fatigue, among others. At times, there may be little or no symptoms. The common risk factors for developing CAD include hypertension, hypercholesterolemia, diabetes mellitus, obesity, sedentary lifestyle, cigarette smoking, stressful life conditions, and family history of CAD.
Aside from the hereditary component, most of the noted risk factors can be improved by lifestyle changes such as eating heart healthy diet, regular exercise, losing weight, smoking cessation, controlling blood sugar, blood pressure, and cholesterol, as well as with medications as needed.
If you develop any of the above symptoms, especially in the setting of having risk factors for CAD, you must immediately seek medical attention for proper evaluation and guidance. Most common initial studies include EKG (electrocardiogram), stress test, and echocardiogram. In addition to the above noted treatment measures, further therapy may also involve coronary angioplasty with stent or open heart bypass surgery.
Artial Fibrillation
Atrial fibrillation (A Fib or AF) is the most common heart rhythm disturbance. Heart rhythm is normally a well regulated electrical activity originating from sinus node, a focus in heart's upper chamber, hence called normal sinus rhythm. This regular electrical impulse conducts down an established circuit, resulting in cyclic heart beats.
AF, on the other hand, is a chaotic rhythm that is overtaken by the tissues of upper chamber called atrium. In the U.S., more than 2 million people are afflicted with AF with nearly 1 out of 10 people over the age of 80. One out of three hospital admissions for arrhythmia is due to AF, costing over $7 billion each year in the U.S. One to two out of 10 strokes are caused by AF as this chaotically fibrillating rhythm can cause stagnant blood flow in the atrium with tendency to form blood clot, which can travel to the brain.
AF can be paroxysmal (temporary and intermittent) or chronic and mostly persistent. When it is temporary, the common causes or associated conditions include excessive alcohol consumption, surgery, during or following heart attack, lung disease such as emphysema and sleep apnea, and thyroid disease. When chronic and persistent, associated conditions may include hypertension, cardiomyopathy (heart muscle disease) with heart failure, heart valve disease, diabetes, and certain congenital heart disease.
Symptoms from AF can vary from severe debilitation with shortness of breath, palpitation and chest pain to little or no symptoms. The treatment approach is to control rate and/or rhythm while the patient is anticoagulated (thinning of blood) to prevent stroke. If medical therapy alone is ineffective in restoring normal sinus rhythm, AF therapies include electrical cardioversion, catheter-based ablation, and open or minimally invasive heart surgeries to target the region where AF originates.
Heart Valve Disease
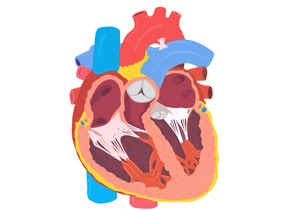
There are 4 heart valves that function as door ways for blood flow between chambers and for great vessels. When these valves either get narrowed with blockage to blood flow or develop inadequate closure with backward leakage of blood flow, one is diagnosed with disease of the involved heart valve(s). When the flow pathology becomes severe, one develops symptoms such as shortness of breath, chest pain, feeling faint, palpitation, and swelling due to fluid retention.
The initial clue to valve disease is a heart murmur during physical examination. The most common tests for this disease are echocardiogram and stress test. If low salt diet and medicine are not effective as initial treatment, the condition may eventually require either repair or replacement with prosthetic valve, most commonly by open or minimally invasive heart surgery. In anticipation for this surgery, cardiac catheterization is usually performed to further confirm this valve pathology and to evaluate for obstructive coronary artery disease prior to the open heart surgery.
Cardiomyopathy

This is a pathology involving the pumping function of heart muscle. It is usually categorized as ischemic or non-ischemic cardiomyopathy. When heart is injured by myocardial infarction (MI or heart attack), this results in ischemic cardiomyopathy with impaired heart function of varying severity. The non-ischemic cardiomyopathy can be caused by a number of conditions. Among the more common causes are long standing hypertension, uncorrected heart valve disease, diabetes, viral infection, advanced kidney disease, and chronic alcohol abuse.
For non-ischemic cardiomyopathy, this condition sometimes improves to normal or near-normal state with appropriate medical treatment. For some, however, the impaired heart function may further deteriorate to cause frequent episodes of heart failure. As there is a higher chance of lethal arrhythmia in this setting as well, placement of ICD (implantable cardioverter-defibrillator) is considered in these patients to help prevent sudden cardiac death. For ischemic cardiomyopathy, treatment of underlying coronary artery disease sometimes improves the heart function while ICD placement is also considered in those with persistently weak heart function.
Heart Failure

Also known as congestive heart failure, this condition occurs when the heart is not able to pump enough blood and oxygen to meet the needs of the body. Common causes are coronary artery disease, cardiomyopathy, untreated heart valve disease, arrhythmia (heart rhythm disturbance), uncontrolled hypertension, chronic lung disease, and congenital heart disease.
Heart failure usually is accompanied by symptoms of shortness of breath, coughing, loss of stamina, and swelling, especially in the ankles and feet with weight gain. When the symptoms are new, the initial diagnostic studies often include EKG (electrocardiogram), echocardiogram, and stress test, as well as full history and physical examination.
Treatment is initiated with appropriate set of medications to control the symptoms and to correct the underlying cause once this is determined. For severe non-ischemic cardiomyopathy, if the pumping function remains markedly impaired, ICD (implantable cardioverter-defibrillator) may be considered to prevent sudden cardiac death from lethal arrhythmia.
Syncope

Syncope simply means passing out or fainting. This can be brought on by several causes, including heart arrhythmia (rhythm disturbance), coronary artery disease (CAD), stroke, dehydration, low blood sugar, or heart valve disease, but the most common type is vasovagal syncope. This is also known as common fainting spells. When the nerves and cardiovascular system lose the usual coordination for normal bodily function, blood vessels dilate or heart rate can slow inappropriately with subsequent drop in blood pressure, causing syncope.
Once more serious conditions such as arrhythmia, CAD, aortic valve disorder, and stroke are excluded, the patient is treated for vasovagal syncope with increased hydration and at times with medication(s). For further confirmation of this diagnosis, tilt testing is occasionally performed.
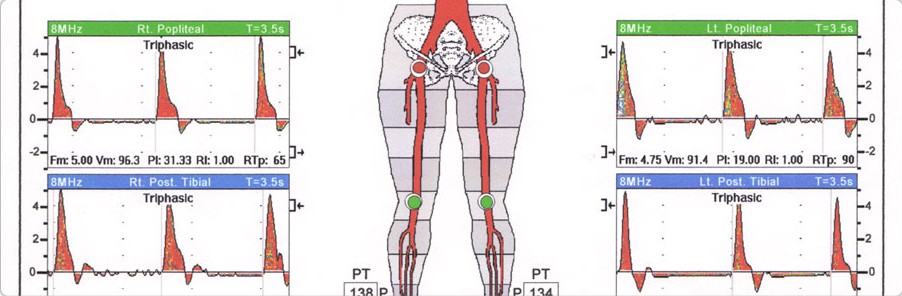
Peripheral Arterial Disease

Similar to coronary artery disease, peripheral arterial disease (PAD) develops by atherosclerotic plaque build up. Most commonly affected regions tend to be legs, arms, neck, and at times gut and kidney arteries. When flow-limiting blockage occurs, the area supplied by the involved blood vessels become ischemic, i.e., oxygen-deprived. If legs are involved, this ischemia is often accompanied by buttock, thigh, or calf pain, which frequently worsens with walking. When this blood flow is severely reduced due to extensive disease, the involved foot can feel cold to touch, and poorly healing wounds may occur with the possibility of gangrene and limb loss if left untreated.
Common risk factors for PAD, like those for coronary artery disease (CAD), include smoking, diabetes, high blood pressure, high cholesterol, and advanced age. One to two out of ten people over the age of 65 are known to have PAD. As there is much higher chance of having concurrent CAD in those diagnosed with PAD, 4 to 5 times increased risk of suffering heart attack or stroke in this population with peripheral arterial disease has been observed. Early diagnosis and treatment of PAD is crucial in these patients.
PAD is usually detected by ABI (Ankle Brachial Index), Doppler ultrasound, and angiography. The focus of treatment is to improve symptoms and to prevent further disease progression. If medications and increasing activity alone are not effective, angioplasty or bypass surgery is the alternative therapeutic option. Life style changes such as smoking cessation, weight loss, and regular exercise can prevent further disease progression.
Cerebrovascular Disease

This is a form of peripheral vascular disease which mostly involves arteries to or within the brain. When the fatty deposits build and block blood flow or form a blood clot in these arteries, stroke or TIA (Transient Ischemic Attack - "mini" or temporary stroke) occurs. As with other peripheral arterial diseases, cerebrovascular disease is often associated with concurrent coronary artery disease. The risk factors include smoking, old age, high blood pressure, high cholesterol, diabetes, and heart rhythm disorder, especially atrial fibrillation.
A blood clot that occludes the artery to the brain causing stroke can occur within or near the brain, or it can travel from other organs such as heart. The event can result in transient or permanent damage of the brain, or death at times.
Among the common symptoms are sudden difficulties with walking, loss of balance, vision changes, difficulty with speech or understanding words, and severe headache with no known cause. Although in some cases, the process of stroke can be interrupted with clot dissolving medication and/or angioplasty if done within a few hours after the symptoms begin, treatment is ineffective in most patients as they tend to present late following the initial symptoms. Prevention is the best therapy for patients at risk for stroke. If any of the above noted symptoms occur, call 911 immediately for best possible outcome with proper treatment.
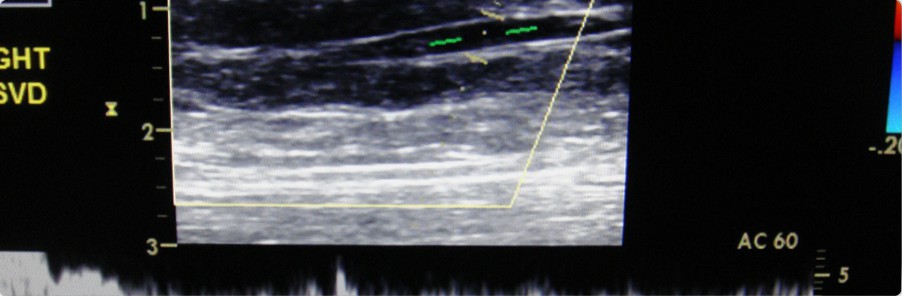
Venous Disease
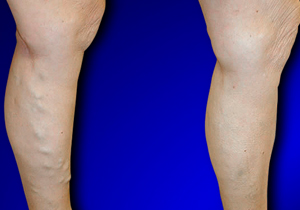
Veins are the blood vessels that return blood to the heart. To overcome the force of gravity, one-way valves exist inside the veins which open to enable the blood return and close to prevent leakage or "reflux" back towards the legs. If these valves become dysfunctional, blood can begin to pool in the leg veins and cause a variety of venous complications over time. It often results in varicose veins, the large, rope-like veins which can cause significant discomfort and complications if left untreated.
While most vein disease can be seen by these superficial varicose veins, in some cases, the diseased veins may be deeper in the body and not be readily visible. Many patients with vein disease experience cramping, aching, burning, itching, tingling, soreness or "restless" legs, especially in the calf muscles.
Venous disease of the legs is one of the most common medical conditions. Approximately half of the population has some form of vein disease. Varicose veins affect approximately 1 out of 4 to 5 adults, nearly half of all people over the age 50, and generally more women than men. Heredity plays an important role as nearly two thirds of all patients with varicose veins have parents with this same condition. Other factors influencing vein disease are pregnancy, obesity, age and jobs that require long periods of standing.
The diagnosis of venous reflux is made with ultrasound evaluation of the superficial veins of legs. Compression stockings are initially tried to help relieve the symptoms. If the discomfort is not entirely relieved by this measure, further treatment options include surgical stripping, sclerotherapy, and more commonly in the recent few years, endovenous laser therapy (EVLT).